IRS ISSUES NOTICE 2015-52 ON CADILLAC TAX IMPLEMENTATION
For taxable years beginning in 2018, the Affordable Care Act (ACA) imposes a 40 percent excise tax on high-cost group health coverage. This tax, also known as the “Cadillac tax,” is intended to encourage companies to choose lower-cost health plans for their employees.
On July 30, 2015, the Internal Revenue Service (IRS) issued Notice 2015-52 to continue the process of developing guidance to implement the Cadillac tax. This notice supplements Notice 2015-16, issued on Feb. 23, 2015.
Notice 2015-52 addresses additional issues under the Cadillac tax, including:
Identification of the taxpayers who may be liable for the excise tax;
Employer aggregation;
Allocation of the tax among the applicable taxpayers; and
Payment of the applicable tax.
The IRS invites comments on these issues and any other issues under the Cadillac tax. Currently, proposed or final regulations have not been issued on the ACA’s Cadillac tax provision. After considering the comments on both notices, the IRS intends to issue proposed regulations under the Cadillac tax.
Taxpayers may not rely on the information provided in Notice 2015-16 or Notice 2015-52.
Overview of the Cadillac Tax
The Cadillac tax provision is found in Internal Revenue Code (Code) Section 4980I. This provision taxes the amount of an employee’s “excess benefit.” The excess benefit is the amount by which the monthly cost of an employee's employer-sponsored health coverage exceeds the annual limitation.
For 2018, the statutory dollar limits are:
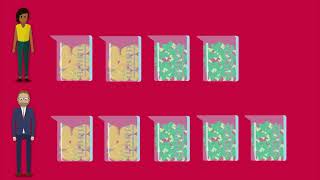
$10,200 per employee for self-only coverage; and
$27,500 per employee for other-than-self-only coverage.
The cost of applicable coverage for purposes of the Cadillac tax is determined under rules similar to those used for determining the COBRA applicable premium.
Who Pays the Cadillac Tax?
The employer will calculate the Cadillac tax amount for each employee’s coverage. The entity responsible for paying any Cadillac tax amount owed is the “coverage provider.” For this purpose, the “coverage provider” is:
The health insurance issuer, in the case of an insured group health plan;
The employer, in the case of a health savings account (HSA) or Archer medical savings account (Archer MSA); and
The person that administers the plan benefits, in the case of any other applicable coverage.
The ACA does not define the term “person that administers the plan benefits,” except that this term includes the plan sponsor, if the plan sponsor administers benefits under the plan.
The IRS is considering two alternative approaches to determining the identity of the person that administers the plan benefits:
Option 1: The person that administers the plan benefits would be the person responsible for performing the day-to-day functions that constitute the administration of plan benefits, such as receiving and processing claims for benefits, responding to inquiries or providing a technology platform for benefits information. The IRS anticipates that this person generally would be a third-party administrator (TPA) for benefits that are self-insured.
Option 2: The person that administers the plan benefits would be the person that has the ultimate authority or responsibility under the plan with respect to the administration of plan benefits (including final decisions on administrative matters), regardless of whether that person routinely exercises that authority or responsibility. The IRS anticipates that this person would be identifiable based on the terms of the plan documents and often would not be the person that performs the day-to-day routine administrative functions under the plan.
Employer Aggregation
For purposes of the Cadillac tax, all employers treated as a single employer under Code Section 414(b), (c), (m) or (o) are treated as a single employer. The IRS invites comments on practical challenges presented by the application of those aggregation rules to the Cadillac tax provision, including the identification of:
The applicable coverage taken into account, as made available by an employer;
The employees taken into account for the age and gender adjustment and the adjustment for employees in high-risk professions or who repair and install electrical or telecommunications lines;
The taxpayer responsible for calculating and reporting the excess benefit; and
The employer liable for any penalty for failure to properly calculate the Cadillac tax imposed.
Calculating the Cost of Applicable Employer-sponsored Coverage
The Cadillac tax applies to “applicable employer-sponsored coverage.” In addition to traditional group health plans, this generally includes coverage under certain HSAs, Archer MSAs, health flexible spending arrangements (FSAs) and health reimbursement arrangements (HRAs).
The amount of any Cadillac tax owed is calculated based on the “excess benefit” with respect to an employee for any taxable period. The excess benefit is the excess, if any, of the aggregate cost of applicable coverage of the employee for the month over the applicable dollar limit for the employee for the month.
Taxable Period
The “taxable period” is generally the calendar year, although the ACA provides that the IRS may prescribe different taxable periods for employers of varying sizes. However, according to Notice 2015-52, the IRS anticipates that the taxable period will be the calendar year for all taxpayers.
Determination Period
Employers will calculate the amount of any Cadillac tax that a coverage provider may owe for a taxable period, and then must notify both the IRS and the coverage provider of the amount of the excess benefit, and the tax must be paid by the coverage provider. Accordingly, the IRS anticipates that employers will have to determine the cost of applicable coverage for a taxable year sufficiently soon after the end of that taxable year in order to enable coverage providers to pay any applicable tax in a reasonably timely manner.
Taking into account the potential approaches in Notice 2015-16 for determining the cost of applicable coverage, as well as other issues with timing implications, the IRS requests comments on the processes expected to be involved in calculating and allocating any excess benefit and the time period necessary to complete these processes.
Passing the Cadillac Tax on to the Employer
In some cases, the IRS anticipates that all or part of the Cadillac tax amount may be passed through to the employer. If the coverage provider does pass through and receive reimbursement for the tax, the excise tax reimbursement will be additional taxable income to the coverage provider.
As a result, the IRS anticipates that the amount the coverage provider passes through to the employer may include both:
The excise tax reimbursement; and
The amount of the additional income tax (the income tax reimbursement).
The ACA provides that any Cadillac tax amount owed may not be taken into account in determining the cost of applicable coverage subject to the excise tax. According to the IRS, this indicates that the excise tax reimbursement should be excluded from the cost of applicable coverage, and it is anticipated that future regulations will reflect this interpretation.
The IRS is also considering whether some or all of the income tax reimbursement could be excluded from the cost of applicable coverage.
Because it may not be feasible to exclude amounts that are not separately billed, the IRS anticipates that coverage providers would be permitted to exclude the amount of any excise tax reimbursement or income tax reimbursement only if it is separately billed and identified as attributable to the cost of the excise tax.
HSAs, Archer MSAs, FSAs and HRAs
The IRS is considering an approach for calculating the cost of applicable coverage for HSAs, Archer MSAs, FSAs and HRAs that are applicable coverage. Under this allocation rule, contributions to account-based plans would be allocated on a pro-rata basis over the period to which the contribution relates (generally, the plan year), regardless of the timing of the contributions during the period.
For example, if an employee elects to contribute to an FSA for a plan year, the employee’s total contributions would be allocated ratably to each calendar month of the plan year, even though the entire amount would be available to reimburse qualified medical expenses on the first day of the plan year.
FSAs with Employer Flex Credits
Certain challenges arise when determining the cost of applicable coverage of an FSA. In general, the cost of applicable coverage of an FSA for any plan year would be the greater of the amount of an employee’s salary reduction or the total reimbursements under the FSA.
The IRS is considering providing a safe harbor to avoid double counting when taking into account salary deferral amounts that are carried over from one year to another year in determining the cost of coverage in both the year of contribution and the subsequent year.
Under this safe harbor, the cost of applicable coverage for the plan year would be the amount of an employee’s salary reduction without regard to carry-over amounts. Unused amounts that are carried over would be taken into account when initially funded by salary reduction, but would be disregarded when used to reimburse expenses in a later year.
This possible safe harbor would be limited to cases in which nonelective flex credits are not available for use in the FSA. To address situations in which nonelective flex credits are available under a cafeteria plan that includes an FSA, the IRS is considering a variation on the safe harbor that would allow an FSA with nonelective flex credits to be valued under the safe harbor in certain situations.
Age and Gender Adjustment to the Dollar Limit
The annual dollar limits for the Cadillac tax can be increased based on the age and gender characteristics of an employer’s workforce, if the cost of providing coverage would be higher for a particular employer’s workforce in comparison to the national workforce.
To establish the age and gender characteristics of the national workforce, the IRS is considering using the Current Population Survey for this purpose, as summarized in Table A-8a, Employed Persons and Employment-Population Ratios by Age and Sex, Seasonally Adjusted (Table A-8a), published annually by the Department of Labor (DOL) Bureau of Labor Statistics (BLS).
To determine the age and gender characteristics of a particular employer’s population, the IRS is considering a requirement that an employer use the first day of the plan year as a snapshot date for determining the composition of its employee population.
The IRS anticipates that it will publish adjustment tables to facilitate the calculation of the age and gender adjustment. A specific seven-step approach is being considered for the development of these tables and the calculation of the age and gender adjustment.
Notice and Payment
The IRS is considering both the form in which the employer must notify the various coverage providers and the IRS of any Cadillac tax due, and the time at which that information must be provided.
The IRS is also considering how calculation errors that affect the cost of applicable coverage could affect multiple coverage providers and how instances of reallocation might be mitigated or avoided.
The ACA does not specify the time and manner in which the excise tax is paid by the coverage provider. The IRS is considering designating the filing of Form 720, the Quarterly Federal Excise Tax Return, as the appropriate method for the payment of the tax. Although Form 720 is generally filed quarterly, under this approach, a particular quarter of the calendar year would be designated for the use of Form 720 to pay the Cadillac tax.
Comment Submissions
The IRS invited comments on the issues addressed in either Notice 2015-16 or Notice 2015-52, and on any other issues under the Cadillac tax provision. Comments should be submitted no later than Oct. 1, 2015. These comments are expected to be used to draft proposed regulations that will be issued in the future.
Reliance
Taxpayers may not rely upon Notice 2015-16 or Notice 2015-52 for guidance regarding the Cadillac tax provision. The IRS also specified that no inference should be drawn from the notice concerning any provision of Section 4980I other than those addressed in the notice or concerning any other section of the ACA or COBRA.