EMBEDDED OUT-OF-POCKET MAXIMUM FOR FAMILY COVERAGE
- stacy174
- May 26, 2015
- 2 min read
Recent guidance from the Department of Health and Human Services (HHS) and the Department of Labor (DOL) provides that, effective for plan years beginning on or after Jan. 1, 2016, non-grandfathered health plans must apply the ACA’s self-only “maximum out-of-pocket” (MOOP) to all individuals, regardless of whether they have self-only or family coverage.
This guidance requires group health plans to embed an individual out-of-pocket maximum in the plan’s family coverage when the family out-of-pocket maximum exceeds the ACA’s out-of-pocket maximum for self-only coverage. This guidance applies to all non-grandfathered group health plans, including self-funded plans and insured plans of all sizes. However, it will likely have the biggest impact on high deductible health plans (HDHPs) because these plans have higher cost-sharing limits.
Embedded out-of-pocket maximum
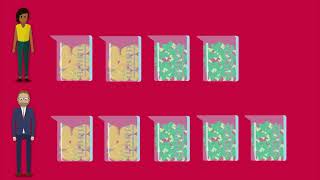
Currently, most group health plans that offer self-only and family coverage have separate out-of-pocket maximums for these levels of coverage, and do not apply the self-only MOOP to individuals who have family coverage. For example, if a plan has a $6,000 MOOP for self-only coverage and a $12,000 MOOP for family coverage, individuals who have family coverage would have their expenses paid at 100 percent for a year, only after the family satisfies the $12,000 MOOP, even if one individual incurred all of the out-of-pocket expenses. According to HHS and the DOL, this type of plan design is no longer permitted for non-grandfathered plans, effective for plan years beginning in or after 2016.
On Feb. 27, 2015, HHS issued its 2016 Notice of Benefit and Payment Parameters under the ACA. In the preamble to this final rule, HHS stated that the ACA’s annual out-of-pocket maximum for self-only coverage applies to all individuals, regardless of whether an individual is covered by self-only coverage or coverage other than self-only (that is, family coverage).
In addition, on May 8, 2015, HHS issued an FAQ explaining how this new guidance affects HDHPs with family deductibles that are higher than the ACA’s cost-sharing limit for self-only coverage.
On May 26, 2015, the DOL issued an FAQ to clarify the application of the new guidance to self-funded and large group health plans and the effective date for the new guidance. In the FAQ, the DOL confirmed that:
Like the ACA’s out-of-pocket maximum for EHB, the requirement that the self-only MOOP be applied to all individuals (regardless of whether they are enrolled in self-only or family coverage) applies to all non-grandfathered group health plans. There are no exceptions for self-funded plans and large group health plans.
This new requirement does not apply to 2015 plan years. It applies to plan years that begin in or after 2016.














Comments