ACA CHANGES OVERVIEW
- stacy174
- Apr 8, 2016
- 4 min read
The Affordable Care Act (ACA) has brought significant changes to the health care industry. This article examines how the new law has affected insured rates, Medicaid, premiums, deductibles and more.
Insured Rates
Since the passage of the ACA, 20 million people have gained health insurance, according to the Obama administration. In 2009 (before the ACA), nearly 49 million people (15.7 percent of the U.S. population) were uninsured. According to a 2015 study by the U.S. Census Bureau, the uninsured rate has dropped to 9.2 percent—the lowest amount in 50 years.
Medicaid
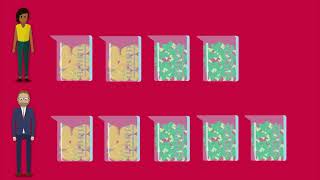
Under the ACA, states have the option of expanding Medicaid to households that make up to 138 percent of the federal poverty line. As of January 2016, 32 states, including the District of Columbia, have elected to expand Medicaid, while 19 states have opted against expansion.
More than 71 million people are enrolled in Medicaid and the Children’s Health Insurance Program (CHIP). This figure marks an increase of 12.3 million people, or 21 percent, since October 2013, when the Health Insurance Marketplace opened.
For states that have opted against expansion, the median income limit in 2016 is 44 percent of the federal poverty level, or an annual income of $8,840 a year for a family of three. Many people living in states that did not expand Medicaid are caught in a “coverage gap”—meaning their incomes are above current Medicaid eligibility limits established by their states, but are below the lowest limit for the Marketplace premium tax credits ($11,770 for an individual in 2016).
Employer Coverage
Despite initial concerns that many employers would drop health coverage as a result of the ACA, most companies have continued to provide health insurance. According to a study by the Kaiser Family Foundation, the percentage of adults under the age of 65 with employer-sponsored health insurance has remained stable for the past five years after steadily declining since 1999.
Many companies view health insurance as an important recruitment and retention tool, especially as the economy has improved. If employers were to drop health insurance, employees would likely expect a higher paycheck or seek employment elsewhere. In addition, employers receive a sizeable tax break for providing health insurance to their employees. While employers’ perceptions could change if health care prices increase dramatically, it appears that employer-sponsored coverage will continue to be offered by the majority of employers in the near future.
Subsidies
Approximately 87 percent of people enrolled in the Marketplace receive a premium tax subsidy. On average, subsidies are $272 per month or $3,264 per year. According to the IRS, 2.7 million taxpayers claimed approximately $9 billion in subsidies when filing their taxes in 2015.
However, about 1.6 million of those taxpayers ultimately had to pay money back to the government because their actual incomes were higher than they had projected when they signed up for a plan on the Marketplace. The average amount repaid was about $800.
Tax Penalties
Approximately 7.5 million Americans paid a penalty for not having health insurance in 2014—the first year in which most Americans were mandated to have coverage under the ACA. The Obama administration initially expected only 2-4 percent of taxpayers to pay the penalty, but in reality, it was about 6 percent.
The average penalty paid among these individuals was $200 per person, and the IRS collected about $1.5 billion from these fines in 2015. The Treasury Department notes, though, that 300,000 people who paid the penalty were likely eligible for a health coverage exemption. These individuals will have the option of filing an amended tax return.
It is possible that tax penalty numbers could decline, since the penalty for not having coverage in 2016 is higher, which may prompt more individuals to purchase health insurance.
Premiums
Premium trends remain a topic of debate among many experts and politicians. Determining premium increases can be difficult due to variations between plans, regions and the people those plans insured.
According to the Department of Health and Human Services (HHS), premiums for standard insurance plans rose by 7.5 percent in 2016. The HHS’ estimates are similar to those from the Kaiser Family Foundation. “Despite the overall growth in Marketplace premiums, the amount many people pay for their coverage could stay relatively flat after their tax credit, but they may have to switch to a different plan in order to take full advantage of that savings,” said Cynthia Cox, associate director of Kaiser’s program on health reform and private insurance.
However, some states and plans have seen dramatic increases. For instance, average monthly premiums for Blue Cross Blue Shield plans increased as much as 49 percent in Minnesota in 2016. Other states, though, experienced less significant premium increases.
On average, premiums have increased by 5.8 percent a year since 2009, compared to the 13.2 percent increase per year between 1999 and 2008. Based on this data, premium increases appear to actually be slowing; however, this number could fluctuate as the market continues to respond to health care reform.
Deductibles
As health care costs continue to rise, more costs are being shifted onto the consumer by way of higher deductibles and copays. High deductible health plans (HDHPs) were present before the ACA, of course, but their popularity in the past few years has grown.
The average deductible for individual and family silver plans on the Marketplace is $2,927 and $6,010. So while subsidies may help lower monthly premiums, high deductibles still make health care unaffordable for many. For instance, a study by the Kaiser Family Foundation found that less than one-fifth of low-income families can afford their high deductibles and only about half of middle-class families can.
In addition, some employers have begun to move towards HDHPs as a way to control rising health care costs and avoid potential penalties associated with the Cadillac tax—helping to further contribute to HDHP enrollment.
Out-of-pocket Maximums
Prior to the ACA, some health plans did not have an out-of-pocket maximum (OOPM) for participants. The ACA requires that all in-network deductibles, copays and coinsurance now be factored into OOPMs for non-grandfathered health plans. Below is a chart showing how the ACA’s OOPMs for non-grandfathered plans have changed over the past three years.
2014 Individual/Family Coverage $6,350/$12,700
2015 Individual/Family Coverage $6,600/$13,200
2016 Individual/Family Coverage $6,850/$13,700
In Summary
Above are just some of the ways in which the ACA has affected the health care industry. Given the novelty of the Marketplace and the constantly evolving nature of the health care industry, these trends are subject to change. For more information on health care reform, contact 360benefits today.














Comments