HOW HEALTH INSURANCE MERGERS COULD CHANGE THE PAYER INDUSTRY
- stacy174
- Sep 2, 2016
- 7 min read
Health Payer Intelligence, September 2, 2016
During the summer of 2015, Aetna and Humana, as well as Anthem and Cigna, started a merger process that would reduce four of the nation's largest insurers down to just two. If the mergers are successful, only three payers would dominate as much as 80 percent of the American marketplace.
While these large companies believe there are significant advantages to consolidating their efforts, industry stakeholders - and the Department of Justice - have reservations about the deals. The DoJ has filed a lawsuit to stop the mergers, citing antitrust concerns, which the four payers will have to fight in court.
Why are these potential health insurance mergers coming under such close scrutiny, and how would they change the payer landscape if they are successfully completed?
Why are payers interested in merging?
All four healthcare payers have claimed that the mergers would benefit consumers. Aetna and Humana believe that their merger would be advantageous for seniors in need of more affordable Medicare Advantage health plans. The payers stated in a press release that there would be more Medicare options throughout more geographies if the deal was to proceed.
Consumers may also benefit from reduced waste, which would decrease costs for policyholders while also bringing more innovation to the market. The payers stressed that reduced costs in the form of lower premiums would be a big draw for continuing the acquisitions.
“Since announcing the transaction, Cigna has remained focused on delivering value to our clients and customers, building on our track record of strong financial results and growing our businesses in the U.S. and abroad,” according to a Cigna statement.
“Cigna has remained strong by continuing to invest in innovative solutions to advance the goals of better health, affordability and personalized experience for our clients and customers and continuing to advance innovative approaches to care management, including expansion in collaborative value-based care arrangements with healthcare professionals across the care delivery spectrum, and designing effective health, wellness and engagement programs for our customers.”
Potential problems with major market consolidation
The Aetna-Humana and Cigna-Anthem health insurance mergers have the potential to create a monopoly on the market, many stakeholders have argued.
The potential for a monopoly on the market means industry groups and politicians have raised antitrust concerns, asserting that there would be much less competition between national payers as well as a reduction in competition from small-to-medium-sized health insurance companies. Essentially, it would harm other payers attempting to compete in the market.
The mergers could also bring harm to the consumer, argued both the American Medical Association (AMA) and the American Hospital Association (AHA). Policyholders may face higher premiums as well as decreased access and choice for their healthcare coverage options.
Also, the health insurance mergers are expected to bring less competition to the insurance market, which would allow the top national healthcare payers to increase their premium prices - a direct negative impact on consumer interests.
A study by the Harvard Business Review asserts that mergers of this kind rarely bring lower premium prices for the end consumer. In fact, the decrease in market competition is likely to only bring higher premiums for the many policyholders that have purchased health plans from these four payers.
Another study conducted by the National Association of Insurance Commissioners (NAIC) shows that these mergers would bring significant payer concentration in a number of states including Georgia, Connecticut and Colorado, which may allow payers to raise their prices without allowing sufficient choice for consumers.
AHA President and CEO Rick Pollack has also stated that these health insurance mergers would severely harm consumers. During testimony in front of the House Judiciary Committee panel, Pollack called for the Department of Justice to address any antitrust regulatory breaches, stating that providers and consumers would be “at risk” if the mergers are allowed to continue.
The American Medical Association also supports the move by the Department of Justice to block these mergers from continuing by enforcing antitrust clauses.
Given the troubling trends in the health insurance market, the AMA believes federal and state regulators must take a hard look at proposed health insurer mergers,” AMA President Steven J. Stack, MD, said in a public statement. “Antitrust laws that prohibit harmful mergers must be enforced and anticompetitive conduct by insurers must be stopped.”
All of these issues were brought to the forefront when the Department of Justice filed a lawsuit against these two health insurance mergers during the summer of 2016.
In June and July of 2016, the Department of Justice received letters from a number of prominent politicians alleging the dangers of the two health insurance mergers and stressing the need to block the acquisitions from taking place.
The letters argued that these mergers would reduce healthcare access and lead to more expensive premiums while, at the same time, hurting smaller payers in the market by reducing competition and creating a monopoly.
As a result of these concerns, the Department of Justice filed a lawsuit against Humana, Aetna, Cigna, and Anthem in order to put an end to these mergers.
Why the Department of Justice is suing
During a press conference on July 21, Principal Deputy Associate Attorney General Bill Baer and Attorney General Loretta Lynch announced the Department of Justice’s decision to pursue a lawsuit against the four health payers. The District of Columbia and 11 other states also filed a petition in court against the Cigna and Humana merger.
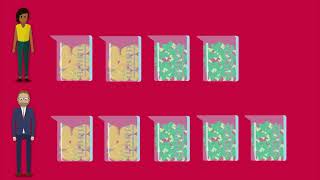
“I’m announcing that the Department of Justice is suing to block both the Anthem-Cigna and Aetna-Humana health insurance mergers,” Attorney General Lynch stated. “These mergers would fundamentally reshape the health insurance industry. They would leave the top five health insurers in just three mammoth companies.”
“Competition would be substantially reduced for hundreds of thousands of families. These mergers may indeed increase the profits of Aetna and Anthem but they would do so at the cost of families, employers, hospitals, and providers,” she added.
Baer added during the press conference that these health insurance mergers would put the entire healthcare system at risk by reducing competition, which would impact seniors and employers.
“These insurance companies are thriving as independent firms. They do not need these deals to survive."
It could also bring problems for doctors and hospitals, since the payers would have more of a monopoly on negotiating provider prices. With a decrease in competition already apparent within the health insurance market, these mergers would only bring more trouble for the industry, said Baer.
“These insurance companies are thriving as independent firms. They do not need these deals to survive". These mergers are likely to harm competition [that would affect consumers] including seniors, working families, employers, as well as doctors and hospitals. Each of these deals poses unacceptable risk to competition,” Baer said.
The competition currently seen between Anthem and Cigna has kept healthcare costs lower, stated Baer, but the health insurance mergers would create financial burdens among seniors on Medicare Advantage plans, according to the Department of Justice review. Along with the upwards trajectory of premium prices that these acquisitions could create, policyholders would also see fewer choices and a decline in benefits if these companies were to consolidate.
“Anthem has had to respond by competing harder and keeping costs down to prevent Cigna from winning away Anthem business. All this competition would be lost if this merger was to take place,” Baer noted.
“Our investigation showed that Aetna’s acquisition of Humana would hurt Seniors with Medicare Advantage plans. This deal would eliminate Humana as a fierce competitor. Seniors would see their choices limited, their benefits reduced, and their premiums go up,” Baer continued. “Our lawsuits aim to protect the many Americans who depend on these four health insurance companies for their coverage.”
US District Judge John Bates set a trial date of December 5 for the DOJ suit against the Aetna and Humana merger. Bates also announced that the final court ruling should take place by the middle of January.
The health payers’ response to the lawsuit
Before the DOJ lawsuit was even filed, Aetna had promised to divest $1 billion in assets to alleviate the concerns around its merger with Humana. However, David Balto, an antitrust attorney based in Washington D.C., wrote in an editorial that the divestitures would not be enough to offset the potential harm if Humana and Aetna consolidate their two companies.
In early August 2015, Aetna and Humana announced that they entered into two separate contracts to sell or divest part of their Medicare Advantage assets to Molina Healthcare. The transactions set aside would total around $117 million and would bring as many as 290,000 Medicare Advantage members across 21 states for Molina Healthcare.
This move is meant to show critics of the health insurance mergers that there would still be some competition preserved within the Medicare Advantage market, which would benefit seniors. Aetna and Humana followed through with these divestitures in order to have more opportunity to continue their plan to consolidate.
By the end of August 2016, Aetna announced that it would be leaving a number of health insurance exchanges due to the financial difficulties of operating in the marketplace as well as the monetary restraint put on by the Department of Justice blocking its merger with Humana.
"This claim was likely an attempt by Aetna to establish a quid pro quo with DOJ; let the merger with Humana proceed, and we will maintain and expand our presence on the exchanges.”
But not everyone is convinced that Aetna’s motives for withdrawing from the exchanges are purely about the difficulties of operating under the ACA framework.
“Aetna is a very large health insurer with substantial resources that it can draw on,” said Balto to HealthPayerIntelligence.com. “It doesn’t need Humana to compete in insurance markets, and DOJ's decision to block the merger likely doesn't impact its ability to participate in the health care exchanges.”
“As others have reported, this claim was likely an attempt by Aetna to establish a quid pro quo with DOJ; let the merger with Humana proceed, and we will maintain and expand our presence on the exchanges,” Balto continued. “DOJ rightly rejected this underhanded attempt to make a deal. The court will do the same. The courts have always held that an anticompetitive merger cannot be justified if there is some other goal that could be met.”
Anthem has also made public statements to bolster its position. The payer said that it seeks to improve the affordability of healthcare benefits along with bringing policyholders high quality services at lower cost. Cigna, however, did not seem as enthused about the merger after the laws suit was filed. The insurer stated in a release that it will likely not close the deal in 2016 but possibly in 2017 “if at all.”
The future for these two health insurance mergers appears uncertain, but it paints a picture where health payers will need to be more vigilant in assessing future consolidation plans with fellow insurers and how it may affect consumer interests. Healthcare payers may need to make more investment in improving marketplace competition and ensuring premium cost control when entering into merger agreements.














Comments